Complementary Treatment for a Patient with Frozen Shoulder
/Studies have demonstrated that conservative treatments may affect the progression of frozen shoulder.
A comprehensive treatment should incorporate a number of rehabilitation strategies based on patient-specific assessment findings including, but not limited to:
• Manual Therapy (neurodynamic mobilization, classic massage, joint mobilizations)
• Acupuncture/ electroacupuncture (local, segmental and distal stimulation sites)
• Education on psychosocial factors (eg. BPS framework of pain, fear avoidance)
• Remedial Loading Programs (eg. static stretching, concentric, eccentric, isometric)
Conservative Care - The Science is Emerging
An improved understanding of the pathophysiology of frozen shoulder may lead to more improved treatment outcomes, and reduce pain, disability and suffering associated with the condition. This post is a brief look at related research, ideally it will serve as a starting point - providing massage therapists and researchers some points of considerations.
Postoperative frozen shoulder is a serious complication after shoulder surgery, with an incidence of 11% (Koorevaar et al. 2017).
Development of a frozen shoulder may also be idiopathic, in either case the theory of recovery phases or complete resolution without treatment for frozen shoulder is unfounded (Wong et al. 2017). In most cases patients benefit from early diagnosis and proper treatment (Yang et al. 2017).
The progression of the frozen shoulder is a complicated process, involving a cascade of molecular and cellular events.
Connective tissue fibrosis and storage of leukocytes and chronic inflammatory cells is thought to play a fundamental role. On going inflammation feeds into a cycle and upregulation of pro-inflammatory cytokine production, namely transforming growth factor beta (TGF-β). This may be further perpetuated by sympathetic dominance of autonomic balance, and neuro-immune activation (Pietrzak 2016).
Impacting Inflammation with Manual Therapy and Gentle Stretching
Persistent inflammation has the potential to interfere with the remodeling of tissue (Rand et al. 2016).
Based on available evidence the mechanisms by which mobilization interrupts the sequelae of pathological healing is most likely not in a single unified response, but as a collection of interconnected adaptive responses within the nervous system and soft tissue structures.
Attenuating Tissue Levels of TGF-β1 - As a therapeutic intervention massage therapy has the potential to attenuate TGF-β1 induced fibroblast to myofibroblast transformation. Recent studies have looked at the effect of modeled massage therapy and mechanical stretching on tissue levels of TGF-β1 (Bove et al. 2016). In this study it was demonstrated that mechanical stretching has the potential to attenuate tissue levels of TGF-β1 and the development of fibrosis. This is potentially impactful in the treatment of frozen shoulder because TGF-β1 plays a key role in tissue remodeling and fibrosis.
Another study suggest that the application of massage induces a phenotype change, prompting the transition of M1 macrophages into the M2 macrophages (Waters-Banker et al. 2014).
Modeled experiments have also demonstrated the impact of stretching on inflammation-regulation mechanisms within connective tissue (Berrueta et al. 2016).
The mechanisms of action are far from conclusive but if clinically translatable, prophylactic massage treatments may inhibit inflammatory processes and affect the development of fibrosis by mediating differential cytokine production.
Pain Management
Other research papers have looked at the neurophysiological mechanisms elicited by manual therapy treatments (Bishop et al. 2015, Vigotsky et al. 2015). Physiological, psychological, and sociological factors interplay in a complex manner, there are a number of possible ways that trigger neuroimmune responses at both the peripheral and central levels.
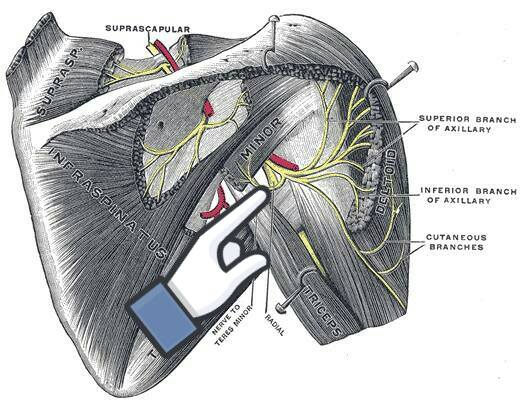
Structures to be aware of when treating frozen shoulder
There are many ways to approach the treatment of frozen shoulder I often treat this area while passively moving the arm through a wide range of motion. Gently stretching the muscles, neurovascular structures and investing fascia of:
• rotator cuff (subscapularis, infraspinatus, teres minor, supraspinatus
• teres major
• triceps brachii
• pectoral muscle group
• serratus anterior
• coricobracialis
• latissimus dorsi
• deltoids
More to Explore
Berrueta, L., Muskaj, I., Olenich, S., Butler, T., Badger, G. J., Colas, R. A., . . . Langevin, H. M. (2016). Stretching Impacts Inflammation Resolution in Connective Tissue. Journal of Cellular Physiology.
https://www.ncbi.nlm.nih.gov/pubmed/26588184
Bishop, M. D., Torres-Cueco, R., Gay, C. W., Lluch-Girbés, E., Beneciuk, J. M., & Bialosky, J. E. (2015). What effect can manual therapy have on a patient's pain experience? Pain Management.
https://www.ncbi.nlm.nih.gov/pubmed/26401979
Bove, G., Harris, M., Zhao, H., & Barbe, M. (2016). Manual therapy as an effective treatment for fibrosis in a rat model of upper extremity overuse injury. Journal of the Neurological Sciences.
http://www.ncbi.nlm.nih.gov/pubmed/26810536 (OPEN ACCESS)
Chapman, M.A., Meza, R., Lieber, R.L. (2016). Skeletal muscle fibroblasts in health and disease. Differentiation.
https://www.ncbi.nlm.nih.gov/pubmed/27282924
Chen, L., Michalsen, A. (2017). Management of chronic pain using complementary and integrative medicine. BMJ.
https://www.ncbi.nlm.nih.gov/pubmed/28438745
Cholok, D., Lee, E., Lisiecki, J., Agarwal, S., Loder, S., Ranganathan, K., Qureshi, A.T., Davis, T.A., Levi, B. (2017). Traumatic muscle fibrosis: From pathway to prevention. J Trauma Acute Care Surg.
https://www.ncbi.nlm.nih.gov/pubmed/27787441
Clewley, D., Flynn, T.W., Koppenhaver, S. (2014). Trigger point dry needling as an adjunct treatment for a patient with adhesive capsulitis of the shoulder. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/24261931
D'Orsi, G.M., Via, A.G., Frizziero, A., Oliva, F. (2012). Treatment of adhesive capsulitis: a review. Muscles Ligaments Tendons J.
https://www.ncbi.nlm.nih.gov/pubmed/23738277
Duchesne, E., Dufresne, S.S., Dumont, N.A. (2017). Impact of Inflammation and Anti-inflammatory Modalities on Skeletal Muscle Healing: From Fundamental Research to the Clinic. Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28789470
Dunn, S. L., & Olmedo, M. L. (2016). Mechanotransduction: Relevance to Physical Therapist Practice - Understanding Our Ability to Affect Genetic Expression Through Mechanical Forces. Physical Therapy.
https://www.ncbi.nlm.nih.gov/pubmed/26700270
Eljabu, W., Klinger, H.M., von Knoch, M. (2016). Prognostic factors and therapeutic options for treatment of frozen shoulder: a systematic review. Arch Orthop Trauma Surg.
https://www.ncbi.nlm.nih.gov/pubmed/26476720
Farrell, K., Lampe, K. (2017). Addressing neurodynamic irritability in a patient with adhesive capsulitis: a case report. J Man Manip Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28855792/
Freitas, S.R., Mendes, B., ... Milanovic, Z. (2017). Can chronic stretching change the muscle-tendon mechanical properties? A review. Scand J Med Sci Sports.
https://www.ncbi.nlm.nih.gov/pubmed/28801950
Gigliotti, D., Xu, M.C., Davidson, M.J., Macdonald, P.B., Leiter, J.R., Anderson, J.E. (2017). Fibrosis, low vascularity, and fewer slow fibers after rotator-cuff injury. Muscle Nerve.
https://www.ncbi.nlm.nih.gov/pubmed/2757128
Hawk, C., Minkalis, A.L., ... Bhalerao, S. (2017). Systematic Review of Nondrug, Nonsurgical Treatment of Shoulder Conditions. J Manipulative Physiol Ther.
https://www.ncbi.nlm.nih.gov/pubmed/28554433
Horst, R., Maicki, T., Trąbka, R., Albrecht, S., Schmidt, K., Mętel, S., von Piekartz, H. (2017). Activity- vs. structural-oriented treatment approach for frozen shoulder: a randomized controlled trial. Clin Rehabil.
https://www.ncbi.nlm.nih.gov/pubmed/28081633
Johnson, A.J., Godges, J.J., Zimmerman, G.J., Ounanian, L.L. (2007). The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J Orthop Sports Phys Ther.
https://www.ncbi.nlm.nih.gov/pubmed/17416123
Koorevaar, R.C., Van't Riet, E., Ipskamp, M., Bulstra, S.K. (2017). Incidence and prognostic factors for postoperative frozen shoulder after shoulder surgery: a prospective cohort study. Arch Orthop Trauma Surg.
https://www.ncbi.nlm.nih.gov/pubmed/28132086
Laumonier, T., & Menetrey, J. (2016). Muscle injuries and strategies for improving their repair. Journal of Experimental Orthopaedics. (Open Access)
https://www.ncbi.nlm.nih.gov/pubmed/27447481
Le, H.V., Lee, S.J., Nazarian, A., Rodriguez, E.K. (2017). Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow.
https://www.ncbi.nlm.nih.gov/pubmed/28405218
Lewis, J. (2015). Frozen shoulder contracture syndrome - Aetiology, diagnosis and management. Man Ther.
https://www.ncbi.nlm.nih.gov/pubmed/25107826
Nanchahal, J., Hinz, B. (2016). Strategies to overcome the hurdles to treat fibrosis, a major unmet clinical need. Proc Natl Acad Sci U S A. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/27342865
Ng, J.L., Kersh, M.E., Kilbreath, S., Knothe Tate, M. (2017). Establishing the Basis for Mechanobiology-Based Physical Therapy Protocols to Potentiate Cellular Healing and Tissue Regeneration. Front Physiol. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/28634452
Page, M. J., Green, S., Kramer, S., Johnston, R. V., Mcbain, B., Chau, M., & Buchbinder, R. (2014). Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews Reviews.
https://www.ncbi.nlm.nih.gov/pubmed/25157702
Page, P., Labbe, A. (2010). Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/21655385
Pietrzak, M. (2016). Adhesive capsulitis: An age related symptom of metabolic syndrome and chronic low-grade inflammation? Med Hypotheses.
https://www.ncbi.nlm.nih.gov/pubmed/26880627
Rand, E., Gellhorn, A.C. (2016). The Healing Cascade: Facilitating and Optimizing the System. Phys Med Rehabil Clin N Am.
https://www.ncbi.nlm.nih.gov/pubmed/27788901
Rawat, P., Eapen, C., Seema, K.P. (2016). Effect of rotator cuff strengthening as an adjunct to standard care in subjects with adhesive capsulitis: A randomized controlled trial. J Hand Ther.
https://www.ncbi.nlm.nih.gov/pubmed/27884497
Ryan, V., Brown, H., Lowe, C. J., & Lewis, J. S. (2016). The pathophysiology associated with primary (idiopathic) frozen shoulder: A systematic review. BMC Musculoskeletal Disorders.
https://www.ncbi.nlm.nih.gov/pubmed/27527912 (Open Access)
Schröder, S., Meyer-Hamme, G., Friedemann, T., ... Briem, D. (2017). Immediate Pain Relief in Adhesive Capsulitis by Acupuncture-A Randomized Controlled Double-Blinded Study. Pain Med.
https://www.ncbi.nlm.nih.gov/pubmed/28371868
Stecco, A., Stern, R., Fantoni, I., Caro, R., & Stecco, C. (2016). Fascial Disorders: Implications for Treatment. Pm&r.
https://www.ncbi.nlm.nih.gov/pubmed/26079868
Struyf, F., Meeus, M. (2014). Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clin Rheumatol.
https://www.ncbi.nlm.nih.gov/pubmed/24374758
Thompson, W. R., Scott, A., Loghmani, M. T., Ward, S. R., & Warden, S. J. (2016). Understanding Mechanobiology: Physical Therapists as a Force in Mechanotherapy and Musculoskeletal Regenerative Rehabilitation. Physical Therapy. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/26637643
Vigotsky, A. D., & Bruhns, R. P. (2015). The Role of Descending Modulation in Manual Therapy and Its Analgesic Implications: A Narrative Review. Pain Research and Treatment. (OPEN ACCESS)
https://www.ncbi.nlm.nih.gov/pubmed/26788367
Waters-Banker, C., Dupont-Versteegden, E. E., Kitzman, P. H., & Butterfield, T. A. (2014). Investigating the Mechanisms of Massage Efficacy: The Role of Mechanical Immunomodulation. Journal of Athletic Training.
https://www.ncbi.nlm.nih.gov/pubmed/24641083 (OPEN ACCESS)
Wong, C.K., Levine, W.N., Deo, K., Kesting, R.S., Mercer, E.A., Schram, G.A., Strang, B.L. (2017). Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy.
https://www.ncbi.nlm.nih.gov/pubmed/27641499
Yang, S., Park, D.H., Ahn, S.H., ... Kim, W. (2017). Prevalence and risk factors of adhesive capsulitis of the shoulder after breast cancer treatment. Support Care Cancer.
https://www.ncbi.nlm.nih.gov/pubmed/27942856